Chemotherapy resistance poses a significant challenge in cancer treatment, hindering the efficacy of drugs and leading to disease progression. Researchers are continuously seeking innovative solutions to address this issue and one promising approach is peptide-drug conjugates (PDCs). These advanced therapeutics aim to enhance the delivery and efficacy of chemotherapeutic agents by utilizing the targeting ability of peptides. By leveraging their potential, PDCs offer new hope in overcoming the barriers posed by resistant cancer cells. This exploration delves into the mechanisms through which PDCs can target cancer cells, bypass drug efflux, and modulate apoptotic pathways, offering a strategic edge in combating chemotherapy resistance. We also examine challenges and future directions to fully integrate PDCs into standard cancer treatment.
Chemotherapy resistance occurs when cancer cells adapt to withstand the effects of anticancer drugs, making treatment less effective. This resistance often results from genetic mutations, altered drug targets, or changes in cellular pathways that affect drug uptake and retention. Cancer cells can develop mechanisms to evade chemotherapy, such as increasing drug efflux pump expression, altering cell death pathways, and enhancing DNA repair capability. As a result, these cells survive and proliferate despite treatment, leading to tumor progression and relapse. Understanding these resistance mechanisms is crucial for developing innovative therapies that can bypass or counteract them. By targeting such mechanisms, peptide-drug conjugate holds promise in providing more effective cancer treatment solutions and overcoming the obstacles posed by chemotherapy resistance.
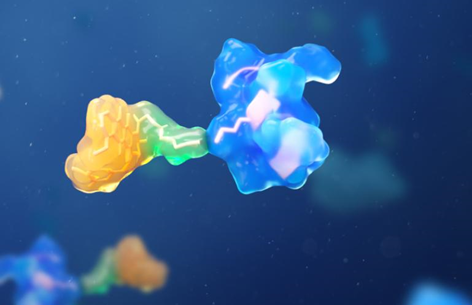
Peptide-drug conjugates (PDCs) emerge as a promising strategy to tackle chemotherapy resistance. They combine peptides’ specific targeting ability with powerful anticancer drugs, allowing for precise delivery to cancer cells. This targeted approach minimizes damage to healthy cells and enhances the drug’s therapeutic effects. By exploiting peptide ligands’ versatility, PDCs can be engineered to bind specific cancer cell markers, directly addressing resistance mechanisms and improving treatment outcomes.
PDCs utilize peptides to achieve targeted delivery of anticancer drugs directly to cancer cells. Peptides can be selected or designed to bind specific receptors or antigens present on the surface of tumor cells but absent on normal cells. This specificity allows PDCs to home in on cancer cells, ensuring that the conjugated drug is released precisely where it’s needed. By concentrating the drug’s action at the tumor site, PDCs increase its efficacy while reducing systemic side effects. Furthermore, this targeted approach can bypass some mechanisms of resistance that arise from non-specific drug distribution, such as drug efflux. The precision of PDCs not only improves the therapeutic index of anticancer agents but also offers a pathway to overcoming the limitations of traditional chemotherapy.
One of the significant hurdles in chemotherapy resistance is the cancer cells’ ability to pump out drugs via efflux transporters, thereby reducing drug accumulation and effectiveness. PDCs offer a solution by facilitating the internalization of drugs into cancer cells, which decreases the likelihood of drug expulsion. The peptide component in PDCs often binds to specific receptors on the cancer cell surface, triggering receptor-mediated endocytosis. This process allows the PDCs to be engulfed and transported into the interior of the cancer cells, bypassing the efflux pumps located on the cell membrane. By circumventing these drug resistance mechanisms, PDCs enhance intracellular drug concentration and improve the overall efficacy of the chemotherapeutic agents against resistant cancer cells.
Cancer cells often evade apoptosis, the programmed cell death process, which is a significant factor in chemotherapy resistance. PDCs can play a critical role in modulating these apoptotic pathways to overcome resistance. By targeting specific receptors linked with survival pathways of cancer cells, PDCs deliver potent anticancer agents that can directly influence apoptotic signaling. This targeted delivery means that the drugs can more efficiently induce apoptosis in cancer cells by activating death receptors or inhibiting survival proteins, thus reversing the cells’ resistant phenotype. The precision of PDCs allows for the activation of apoptosis with minimal impact on healthy tissue, offering a therapeutic advantage in reinstating cancer cell sensitivity to chemotherapy and potentially resulting in better patient outcomes.
While PDCs offer promising strategies, there are challenges such as optimizing stability, bioavailability, and integrating PDCs into existing treatment protocols. Future research should focus on these areas to maximize their clinical potential and ensure these novel therapeutics can be effectively used in standard cancer care.
The stability and bioavailability of PDCs are critical factors influencing their efficacy in clinical settings. Enhancing PDC stability ensures that these conjugates reach their target before degrading or losing their therapeutic activity. This can be achieved through various chemical modifications of the peptide or the linkers that connect the peptide to the drug. Stabilizing the PDCs protects the drug from premature release or breakdown, ensuring it remains intact until it reaches the target cells. Improving bioavailability is also essential; it involves ensuring the PDCs can be efficiently absorbed and circulated in the body to reach the target tumor cells at therapeutic concentrations. Novel formulation techniques and the use of delivery systems like nanoparticles or liposomes may enhance the stability and bioavailability of PDCs, making them more viable for clinical use.

For PDCs to become a staple in cancer treatment, they must seamlessly integrate into existing treatment regimens. This integration requires robust clinical trials to establish their safety, efficacy, and potential synergies with traditional therapies. Combining PDCs with chemotherapy or immunotherapy may enhance overall treatment outcomes by targeting multiple cancer pathways simultaneously. Oncologists need clear guidelines on how to incorporate PDCs into therapy plans, possibly in cases where resistance is identified or anticipated. Additionally, healthcare systems must be equipped to handle the production and storage of PDCs, ensuring consistent quality and availability. The successful integration of PDCs into standard care will rely on interdisciplinary collaboration and continued advancements in clinical research and patient management strategies.
PDCs provide an exciting opportunity to combat chemotherapy resistance by leveraging targeted delivery, bypassing cellular resistance mechanisms, and efficiently triggering cell death in resistant cancer cells. Although challenges remain in optimizing their stability, bioavailability, and clinical integration, ongoing research and development hold promise for their future applications in cancer treatment. As PDC technology evolves, it may significantly enhance the effectiveness of cancer therapies, offering new hope for patients facing resistant tumors. By continuing to explore and refine these strategies, the medical community moves closer to more effective and personalized cancer treatment solutions, potentially transforming the landscape of cancer therapeutics.